Conventional treatment for periodontitis uses scaling and root planing to physically remove plaque below the gum line and reduce harmful bacteria. However, without ongoing control, these bacteria can quickly repopulate the pockets and cause the disease to return.
NEED GAP OF THERAPY
Limitations of Conventional Antibiotics in Dentistry
- Non-Specific Action: Antibiotics target a broad range of bacteria, including beneficial oral microbiota, leading to dysbiosis and imbalance in the oral microflora.
- Antibiotic Resistance: The overuse of antibiotics in dental care contributes to the global rise in antimicrobial resistance (AMR), reducing their long-term effectiveness.
- Short-Term Effects: Antibiotics often provide temporary relief from bacterial infections without addressing the root cause, such as biofilm formation or inflammation.
- Side Effects: Conventional antibiotics can cause adverse effects such as gastrointestinal disturbances, allergic reactions, or opportunistic infections (e.g., candidiasis).
Challenges in Maintaining Balanced Oral Microflora:
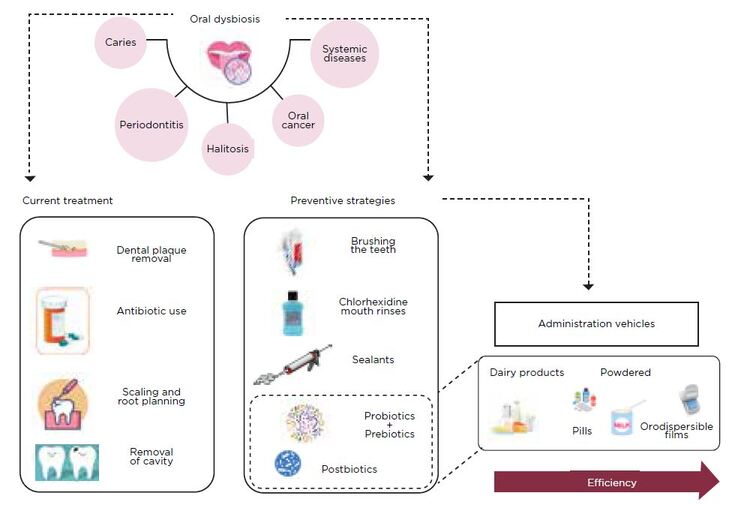
- Oral Dysbiosis: Factors such as poor oral hygiene, diet, and antibiotic use disrupt the natural balance of oral microbiota, promoting the growth of pathogenic bacteria.
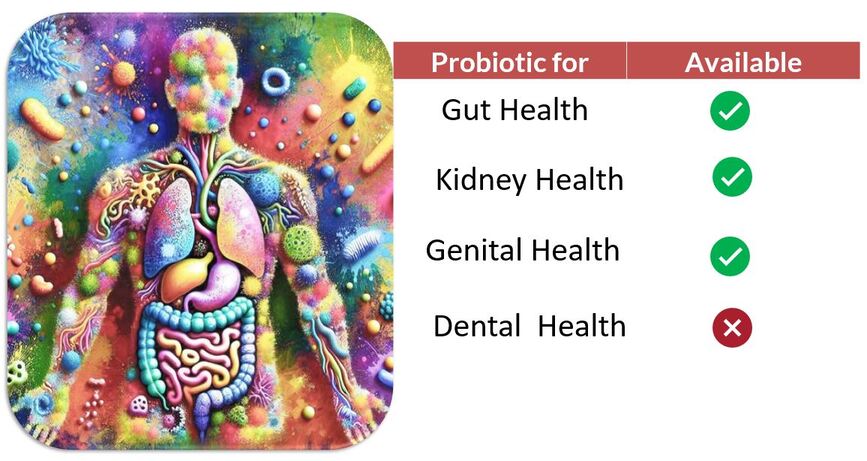
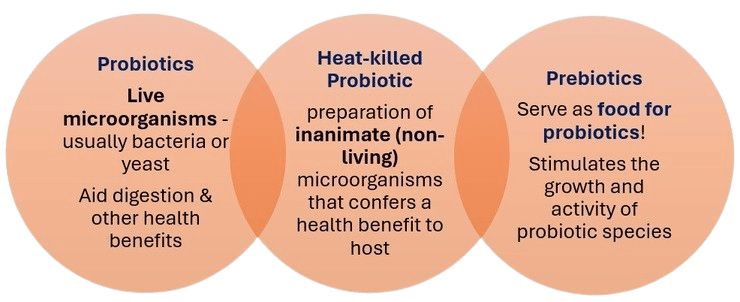
Limitations of Prebiotics and Probiotics
Prebiotics
- Dependency of existing microbiota: Prebiotics require a healthy microbiota to be effective, limiting their use in dysbiotic conditions
Probiotics
- Survivability Issues: Probiotics may not survive gastric acid, bile, or harsh oral conditions, reducing efficacy.
- Storage Sensitivity: Probiotics require specific storage conditions for viability.
- Risk of Infection: In rare cases, probiotics can cause bacteremia in immunocompromised individuals.
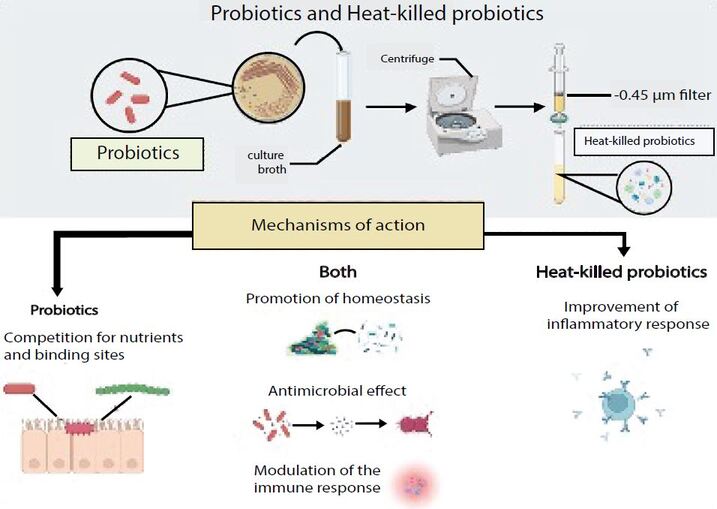
What is heat killed probiotic?
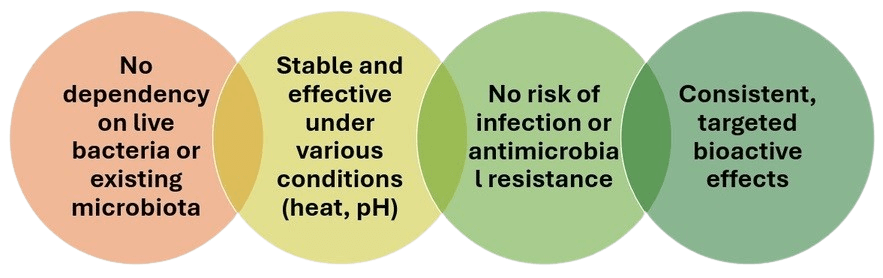
Why heat killed probiotic?
Role of L.paracasei GMNL-33 in oral health
The Lactobacillus paracasei species includes non-motile, non-spore-forming, rod shaped, facultative anaerobic lactic acid bacteria (LAB) that populate several niches, from fermented foods to host-associated microenvironments. The cell wall of lactobacilli is made up of peptidoglycan, a type of carbohydrate protein complex that helps to give the cell its shape. The cell wall also contains lactic acid, which helps to protect the bacterium from acidic environments. The cytoplasm of lactobacilli is clear and contains a small amount of DNA. In addition to the cell wall and cytoplasm, lactobacilli also have a thin layer of slime that covers their surface. This slime layer helps the bacteria to attach to surfaces and protects them from dehydration. The strain stains Gram-positive.

Lactobacillus paracasei GMNL–33, which is effective in reducing dental plaque and gingival formation by inhibiting associated oral pathogens such as Streptococcus mutans, Porphyromonas gingivalis, and Prevotella intermedia.